Beautiful Plants For Your Interior

David A. Ansell, M.D., M.P.H., Kaitlyn Fruin, M.D., Redia Holman, Ayesha Jaco, M.A.M., Bich Ha Pham, J.D., and David Zuckerman, M.P.P.
In 2016, Rush University System for Health, an academic health system in Chicago, adopted an anchor strategy to tackle the 16-year life-expectancy gap between Chicago’s West Side and the Loop (see map). An anchor strategy is a place-based business approach to building community health and wealth by means of local hiring, investing, purchasing, and community engagement. The concept was first articulated by the Aspen Institute in 2001 with a focus on the community-building potential of universities but has recently gained momentum in health care.1 Among the largest property owners, employers, and purchasers in their regions, anchor health and educational institutions can stimulate local economic growth using their everyday business practices.
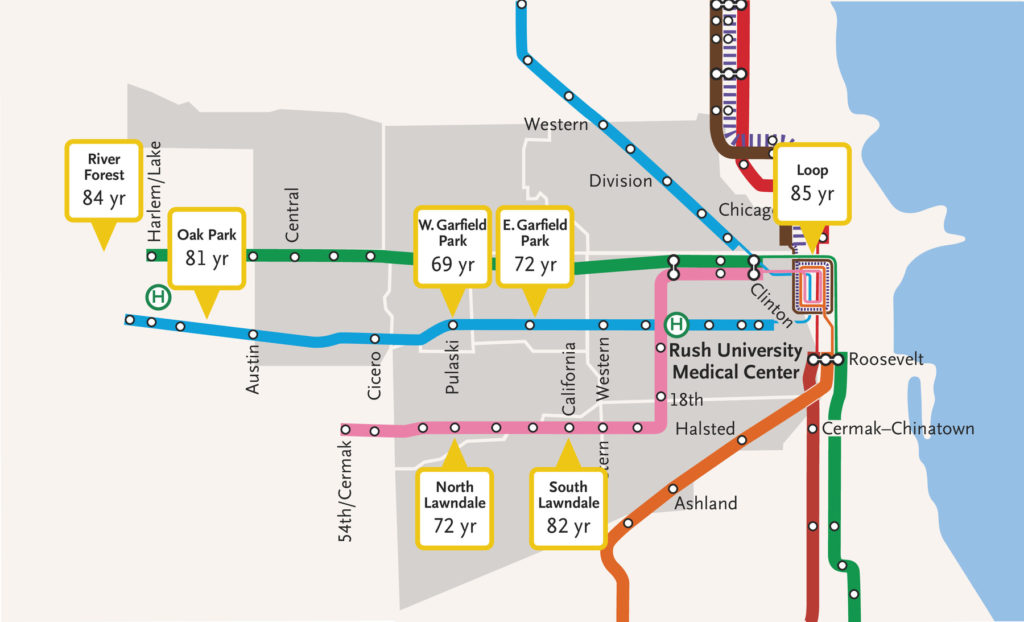
In Rush’s case, a 2016–2019 Community Health Needs Assessment (CHNA) illuminated deep-seated structural racial health inequities that required efforts beyond traditional health care delivery and community engagement. We identified structural racism and economic deprivation as among the root causes of neighborhood life-expectancy gaps and in 2017 launched the anchor strategy to leverage Rush’s position as a large business in addressing these social drivers of population health.
Later in 2017, Rush and 10 other health care systems joined the Democracy Collaborative, an economic-development think tank, to launch the national Healthcare Anchor Network (HAN). HAN is an independent 501(c)(3) organization that now has 75 health care system members; these members collectively spend more than $150 billion per year, purchase $75 billion worth of goods and services per year, hold investment portfolios totaling more than $500 billion, and employ more than 2 million people.
Rush’s anchor strategy offers an evolving case study in place-based population health investments.2,3 An internal anchor-strategy committee comprising leaders from human resources, finance, construction, community engagement, and supply-chain operations sets annual targets for local hiring, participation in career pathways, investing, purchasing, and volunteering, all of which are included in a corporate dashboard. We decided that a critical step in this strategy was to designate employees, many of whom live in West Side neighborhoods, as the “first community.” We conducted internal “listening sessions” and created a West Side employee resource group so that employees could inform the initiatives.
Internal analyses showed that employees living in neighborhoods with low life expectancy had the highest rates of financial distress, as measured by lack of full participation in the 403(b) retirement plan, by emergency withdrawals from their retirement accounts to address such problems as evictions, or by garnishment of wages. Efforts to improve wealth building among Rush employees included the creation of new career pathways and pension reforms4 that resulted in a 46-percentage-point increase in the proportion of employees with the highest level of 403(b) matching, from 34% in 2017 to nearly 80% in 2021. Currently, 88% of Rush employees earn more than the regional living wage.
In 2018, Rush was joined by 5 other health systems — AMITA (now Ascension) Health, Cook County Health, Lurie Children’s Hospital of Chicago, Sinai Chicago, and University of Illinois Health — to establish West Side United (WSU), a racial-equity collaborative aligning investments in economic development, education, health care, and the built environment to benefit Chicago’s 500,000 West Side residents. The combined assets of these health care anchors are larger than those of any Illinois corporation and create potential for major collective impact. Under the umbrella of WSU, the 6 health systems conducted “listening tours” to identify and prioritize community needs. Community leaders sit on an executive leadership council that has equal representation from the community and the hospitals. Ongoing input is obtained through regular community meetings.
In 2020, Rush and WSU pivoted to respond to the disproportionate burden of the Covid-19 pandemic on Chicago’s Black and Latinx communities. The mayor’s office asked WSU, which had built a reputation as a trusted community convenor, to colead a citywide Racial Equity Rapid Response Team (RERRT) coordinating the community-level pandemic response with community leaders, the health department, and health care providers. Rush was asked to colead the health care workgroup of the RERRT. WSU managed the distribution of $6.9 million in relief dollars to more than 35 community organizations in 23 Chicago communities. In response to the racial disparity in Covid-19 mortality and to the murder of George Floyd in May 2020, the RERRT had 36 health care members publish a statement declaring racism a public health crisis and outlining commitments to address systemic racism — a statement that was subsequently adopted by 40 HAN health systems nationwide.
Since 2018, WSU members and the American Medical Association have invested $10.8 million through community development financial institutions to finance businesses, nonprofits, and affordable housing; raised $3 million to establish four health care career pathways; launched interventions targeting hypertension and maternal and infant outcomes in West Side hospitals, clinics, and community-based organizations; hired more than 2000 West Side employees; and raised $1.9 million to support local businesses. WSU’s small business accelerator offers business-development support to 150 West Side businesses and 60 community-based organizations.
Shared activities of WSU hospitals — such as identifying West Side vendors, allocating $34 million in contracts to West Side businesses in 2021, hosting hiring fairs, and codeveloping career pathways — enable collective wealth-building efforts. Concordance, a supply-chain integrator that supplies Rush and other health systems, has located its 165,000-square-foot warehouse facility on the West Side, and the terms of its contract with Rush require local hiring targets. Rush is a capital sponsor for a planned $50 million community-led and -owned health and wellness project, “Sankofa Wellness Village,” in Garfield Park, a West Side neighborhood with low life expectancy. Other similar community capital investments supported by other WSU health systems in Chicago and by HAN health systems elsewhere include the notable contributions of CommonSpirit and Kaiser to social-impact investment nationwide.
The anchor-strategy movement faces several challenges, but two loom large: funding and outcome measurement. Anchor-institution champions must secure institutional support and funding for operations, evaluation, and meaningful community engagement. Health systems, particularly in an era of shrinking margins, may balk at infrastructure investments for an anchor strategy. Although the Affordable Care Act mandated completion of CHNAs and Community Health Improvement Plans (CHIPs), hospitals were not provided additional resources to invest in innovative public health initiatives. We believe that just as the Health Information Technology for Economic and Clinical Health (HITECH) Act provided financial incentives for adoption of electronic health records, federal legislation is needed that offsets the costs of adoption of meaningful anchor strategies.
Other critical questions center on how best to monitor outcomes. At Rush, and for many other HAN members, CHNAs and CHIPs provide a roadmap for evaluating the success of the anchor strategy. HAN has developed a dashboard of health and socioeconomic metrics that form the basis of ongoing performance measurement. Similarly, WSU monitors progress using a public-facing dashboard that tracks outcomes across four domains: health and health care, economic vitality, educational attainment, and neighborhood built environment. Metrics include local hiring and career pathways, purchasing, investing, public health, and community wealth building. But anchor strategies may take years to measurably improve population health, particularly after the declines in life expectancy seen during the Covid-19 pandemic. Methods such as social-return-on-investment analyses have shown promise for capturing the broader social, environmental, and economic benefits of anchor investments.5 Federal and philanthropic grant funding is necessary to support evaluations of existing anchor initiatives to distinguish which ones have the highest social return on investment.
Despite these challenges, an anchor strategy can be an effective health care institution approach to address place-based, racial, economic, and other structural inequities that drive population health and wealth.4
Disclosure forms provided by the authors are available at NEJM.org.
This article was published on January 7, 2023, and updated on January 11, 2023, at NEJM.org.
Author Affiliations
From the Department of Internal Medicine (D.A.A.) and the Care Management Program (R.H.), Rush University Medical Center, and West Side United (A.J.) — both in Chicago; the Department of Internal Medicine, Ronald Reagan UCLA Medical Center, Los Angeles (K.F.); and the Healthcare Anchor Network, Washington, DC (B.H.P., D.Z.).
Supplementary Material
| Disclosure Forms | 473KB |
