Beautiful Plants For Your Interior

Frederica Perera, Dr.P.H., Ph.D., and Kari Nadeau, M.D., Ph.D.
The combustion of fossil fuels (coal, petroleum [oil], and natural gas) is the major source of both air pollution and the greenhouse-gas emissions driving climate change. The fetus, infant, and child are especially vulnerable to exposure to air pollution and climate change, which are already taking a major toll on the physical and mental health of children. Given the frequent co-occurrence of various fossil-fuel exposures, their interactions and cumulative environmental impacts are a growing concern. All children are at risk, but the greatest burden falls on those who are socially and economically disadvantaged. Protection of children’s health requires that health professionals understand the multiple harms to children from climate change and air pollution and use available strategies to reduce these harms.
Consequences of Fossil-Fuel Emissions
Figure 1.
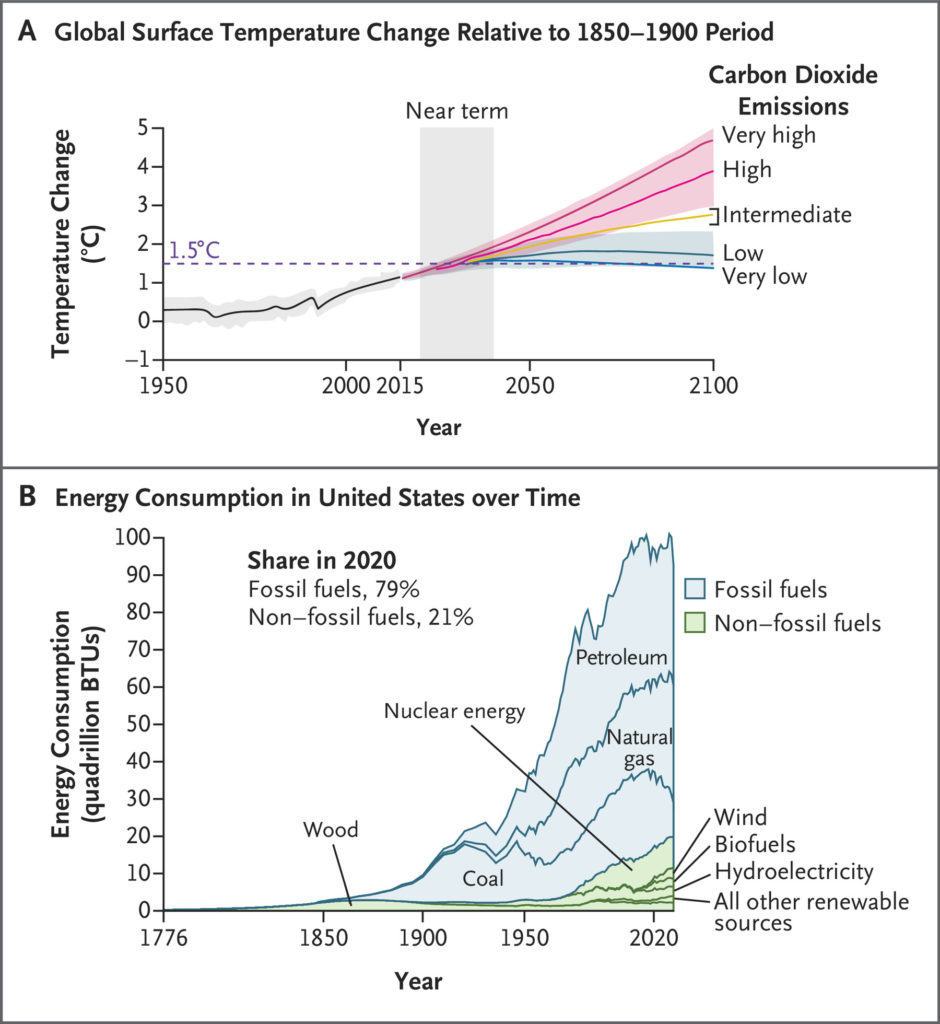
Emission Sources and Trends.
Panel A shows the trends in carbon dioxide emissions since 1950. Global-warming thresholds of 1.5°C and 2.0°C will be exceeded unless deep reduction in carbon dioxide and other greenhouse-gas emissions occurs in the coming decades. The bracket indicates a predicted trajectory of temperature increase (2.5 to 2.9°C) by 2100 on the basis of current policies and action to reduce greenhouse-gas emissions.3 Adapted from the Intergovernmental Panel on Climate Change (https://www.ipcc.ch/report/ar6/wg1/downloads/outreach/IPCC_AR6_WGI_Press_Conference_Slides.pdf. opens in new tab). Panel B shows energy consumption of both fossil fuels (coal, petroleum [oil], and natural gas) and non–fossil fuels (wood, nuclear energy, wind, biofuels, hydroelectricity, and other renewable sources) in the United States throughout its history (from 1776 to 2020). Since 2020, petroleum use has increased (data not shown). Adapted with permission from the U.S. Energy Information Administration (https://www.eia.gov/todayinenergy/detail.php?id=48576. opens in new tab). BTU denotes British thermal unit.
Worldwide, in recent years, billions of tons of carbon dioxide and more than 120 million metric tons of methane, the two key greenhouse gases, have been emitted annually into the atmosphere from the production and burning of fossil fuels for energy and transportation.1 Carbon dioxide emissions from fossil fuels have risen sharply in the past 70 years, reaching 35 billion metric tons of carbon dioxide emitted in 2020, as compared with just 5 billion metric tons in 1950.2 Figure 1 shows the need for deep reductions in greenhouse-gas emissions and the sharp increase in fossil-fuel–based energy consumption in the United States.
Largely as a result of fossil-fuel emissions, the average surface temperature of the earth has increased by approximately 1.1°C (2°F) since preindustrial times.4 The Intergovernmental Panel on Climate Change has concluded that urgent action is required in order to limit global warming to 1.5°C (2.7°F) above preindustrial levels and to minimize the most catastrophic consequences.4 We are on track to reach this threshold within the next two decades and, with current climate policies, to have an increase in temperature of 2.5 to 2.9°C above preindustrial levels by the end of the century.3 Although an increase of more than 1.5°C appears to be locked in within the next two decades, we can change the trajectory after that by taking immediate action.4,5 Citing the devastating effects on health, 200 health journals, including the Journal, recently called on world leaders to take emergency action on climate change.6
The combustion of fossil fuels has created a parallel crisis of air pollution, because the burning of these fuels releases massive amounts of airborne fine respirable particles with an aerodynamic diameter of 2.5 μm or less (PM2.5), sulfur dioxide, nitrogen oxides, polycyclic aromatic hydrocarbon (PAH), mercury, and volatile chemicals that form ground-level ozone. One billion children worldwide are exposed to very high levels of air pollution.7 Fortunately, solutions are now available to substantially reduce, and in some cases eliminate, these emissions.8
Vulnerabilities of Children to Effects of Climate Change
Figure 2.

Susceptibilities in Fetuses, Infants, and Children Associated with Climate Change and Exposures.
Adapted from Haines and Ebi.12 Shown are examples of potential exposure pathways, susceptibilities, and potential health outcomes linking climate change with children’s health. PTSD denotes post-traumatic stress disorder.
The fetus, infant, and child are uniquely vulnerable to climate-related environmental impacts and air pollution owing to a host of biologic and behavioral factors.9-11 The speed of development and the elaborate developmental programming during these stages confer high susceptibility to disruption by toxic chemicals and other stressors. In addition, the biologic defense mechanisms for detoxifying chemicals, repairing DNA damage, and providing immune protection are immature in the infant and child, thus heightening their vulnerability to psychosocial stress and physical toxicants (Figure 2).
To support their rapid growth, the infant and child have greater nutritional and fluid requirements than adults and, therefore, a greater vulnerability to food and water supply disruptions. Infants and children breathe more air relative to their body weight than adults, which increases their exposure to air pollutants, and their narrower airways are vulnerable to constriction by air pollution and allergens.
Infants and children are more vulnerable than adults to severe heat because of their compromised thermoregulatory function at extreme temperatures13 and their dependence on care by adults who may be unaware of the risks, as when infants left in cars have died from the heat. Children also spend more time outdoors engaged in physical activity than adults.
Children are especially vulnerable to the effects of displacement due to weather disasters; they are prone to physical injury and psychological trauma as a result of being forced to leave their homes. Finally, children have a long remaining lifetime during which early illnesses such as asthma or mental health conditions may persist, affecting health and functioning in adulthood.
Effects of Climate Change
Table 1.
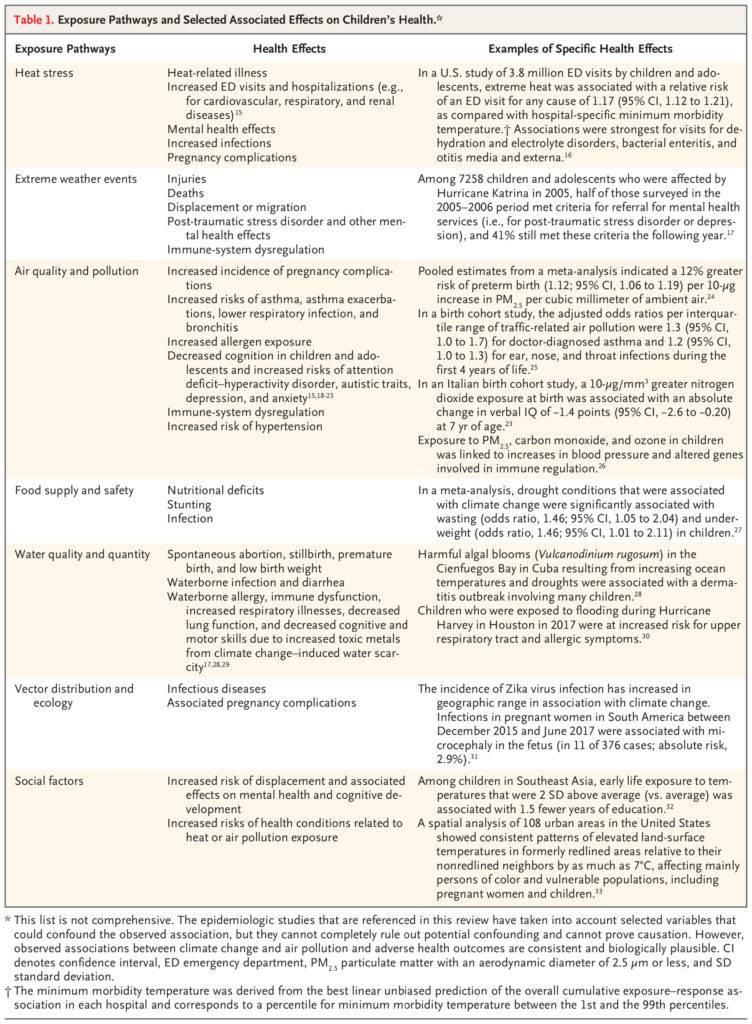
Exposure Pathways and Selected Associated Effects on Children’s Health.
Climate change is a threat multiplier for infants and children,14 acting through multiple pathways. Climate change has worldwide effects on health; nearly every child around the world is considered to be at risk from at least one climate hazard (Figure 2 and Table 1).7
EXTREME HEAT
Heat waves (defined as ≥2 days of unusually hot weather) are increasing in frequency and intensity; modeling indicates that some heat waves would be extraordinarily unlikely to occur in the absence of climate change.34 Exposure to heat waves during in utero development is associated with increased risks of preterm birth and low birth weight; hyperthermia and death among infants; and heat stress, kidney disease, and other illnesses among children.16,35 In the United States, heat-related illness is a leading and increasing cause of death and illness among student athletes. Studies suggest that heat associated with climate change has adverse effects on the mental health of children and adolescents, including increased mental health–related emergency department visits; such extreme heat also affects children’s ability to learn.36,37
CLIMATE-INTENSIFIED EXTREME EVENTS
Climate change has intensified major floods and hurricanes, which have caused drowning, physical injury, and traumatic stress in children.34 Risks from extreme weather events are greatest in low- and middle-income countries. Climate-related events have already contributed to more than 50 million children worldwide being forced to leave their homes.38,39 In the United States, however, more than 900,000 displacements, many of them involving children, occurred in 2020 as a result of disasters.40 Children in low-income communities and communities of color are disproportionately harmed by these events. Effects may include disruption of education and mental health problems such as post-traumatic stress disorder and depression.41
WILDFIRE SMOKE AND AEROALLERGENS
As a result of climate change, the western United States has had dramatic increases in forest fires in recent years.42 An estimated 7.4 million children in the United States were exposed to lung-damaging wildfire smoke every year between 2008 and 2012.42 This number has increased in recent years as large forest fires in the western United States have become even more frequent. Exposure to wildfire smoke in utero has been linked to decreased birth weight and preterm birth; exposures in childhood are associated with asthma exacerbations, wheeze, pneumonia, and bronchitis.43
Children are also having more allergy and asthma attacks from increased levels of airborne pollen as a result of higher temperatures and rising levels of carbon dioxide, which have resulted in longer growing seasons and increased pollen production.44-46 The proliferation of mold in homes from excess moisture due to heavy rains and flooding, as occurred in the New Orleans area during Hurricanes Katrina and Rita in 2005, can trigger an asthma attack regardless of whether the child has a mold allergy.46
DECREASED FOOD AND WATER SUPPLY AND SAFETY
Droughts that are related in part to climate change have affected Central and South America, Afghanistan and other parts of Asia, Australia, sub-Saharan Africa, and the southeastern United States.34 In developing countries, the resulting food insecurity has led to a sharp increase in malnutrition, which has caused stunting of children’s physical and mental development, with associated behavioral and cognitive problems. In addition to the environmental impacts of climate-related drought on the food supply itself, increasing concentrations of carbon dioxide have been linked to a reduction in the nutritional quality of major cereal crops.12
Risks associated with food and water safety are experienced worldwide. Children, especially infants, are particularly susceptible to gastrointestinal infection caused by bacterial pathogens such as salmonella in food and water; these infections are more frequent at higher ambient temperatures that promote bacterial replication.47 Children are also more susceptible than adults to cholera and other infectious diarrheal diseases owing to crop and water contamination from storms and floods.48
CHANGE IN VECTOR ECOLOGY
Climate change is associated with increased risks of several vectorborne diseases, including malaria, dengue, Zika virus infection, and Lyme disease, in certain regions owing to changes in the duration of the transmission season and the geographic spread of the disease vectors.49 The geographic ranges of the species of mosquitoes that carry malaria (anopheles) and dengue (aedes) have expanded because of warmer temperatures. The effect on health is greatest among children in tropical regions; however, small local outbreaks of dengue have been seen in Florida, Hawaii, and Texas.50 The aedes mosquito is also the primary carrier of the Zika virus, which was responsible for the 2015–2016 outbreak in the Americas, including travel-associated cases in the United States.51 Cases of local transmission of Zika virus occurred in Florida and Texas in the 2016–2017 period. Zika virus infection during pregnancy can cause microcephaly, severe brain malformation, and other birth defects.
The United States has also had a marked increase in the incidence of Lyme disease, with the highest rates occurring among children.52 Michigan, Minnesota, New York, Virginia, and western Pennsylvania have all reported an increase in the number of cases of Lyme disease over the past few decades.53
Effects of Air Pollution
Air pollution is a well-known trigger of asthma attacks in children with the disease and is now understood to be a cause of asthma.54 It is also a risk factor for respiratory infections, bronchitis, and impaired lung growth and function.55 A study showed that children with higher exposure to air pollution had more severe asthma symptoms and lower levels of regulatory T cells — factors that play a critical role in controlling allergic diseases such as asthma — than children from a less-polluted area.56
Air pollution is strongly associated with increased risks of infant death and adverse birth outcomes.9 Worldwide, an estimated 2 million preterm births in 2019 were attributed to ambient PM2.5 exposure.24 Although most of these preterm births occur in lower- and middle-income countries, PM2.5 exposure is a recognized risk factor for preterm birth and low birth weight in the United States.57 These birth complications confer increased risks of lower respiratory infections, other infectious diseases, and asthma in childhood, as well as long-term intellectual disabilities.
Prenatal and postnatal exposure to various air pollutants has also been associated with reduced cognition, attention problems, attention deficit–hyperactivity disorder, and autistic traits in childhood.18,58 Studies have shown structural and functional changes in the brains of children who had elevated exposure to air pollutants before birth or during childhood.19,59
Recent epidemiologic research indicates that air pollution is also a risk factor for mental health conditions in children and adolescents. For example, lifetime exposure to traffic-related air pollution in Cincinnati was associated with depression and anxiety symptoms in 12-year-old children.20 In a London-based cohort, children who were exposed to higher levels of outdoor air pollution had increased odds of major depressive disorder at 18 years of age.22
Interactions of Air Pollution and Climate Change
Environmental and epidemiologic data indicate that air pollutants and climate change interact to affect children’s health. Joint occurrence of air pollution, heat, and other climate-related changes has led to worse air quality. Air stagnation and higher temperatures accelerate the formation of ozone, which is associated with respiratory illness in children and with preterm birth. Concentrations of PM2.5 have increased in some areas because of changes in temperature, precipitation frequency, and air stagnation due to climate change. Wildfires, which have been made more frequent and severe by climate change, release vast amounts of particulate matter, PAH, and black carbon, thus adding to the ambient load from fossil-fuel burning. In addition, air pollutants can increase allergen absorption in the lungs and promote sensitization of the airway.60
There is evidence of a synergistic effect of heat and air pollution on the incidence of hospitalization related to childhood asthma.61 More studies on child health outcomes are needed; however, a large epidemiologic study showed a synergistic effect of prenatal exposure to heat and air pollution on the risk of preterm birth.62
Concurrent exposure to climate hazards and unsafe air quality is common. An estimated 850 million children — or 1 in 3 children worldwide — live in areas where at least four climate and environmental shocks, such as severe drought, flooding, air pollution, and water scarcity, overlap.63 Therefore, cumulative effects are likely, such as when children have concurrent exposure to air pollution, extreme temperatures, food insecurity, and social stress from climate change.
Of particular concern are the cumulative effects of air pollution and climate change on mental health. Adverse experiences in childhood, such as disasters and displacement, not only raise the short-term risk of mental disorders but also confer a lasting vulnerability to anxiety, depression, and mood disorders in adulthood.64 Even in the absence of direct experience of effects of climate change, stress due to the awareness of climate change and its effects (termed climate change anxiety) can increase the risk of mental health problems among children and young people. In a survey across 10 countries, nearly 60% of young persons said that they felt very worried or extremely worried about climate change; more than 45% said that their feelings about climate change negatively affected their daily lives.65
Disparities
All children are at risk from air pollution and climate change, but there are substantial inequities according to income and race. Disparities are most obvious between higher- and lower-income countries but are also evident within the United States, where children in low-income communities and in certain racial and ethnic groups, such as Black and Hispanic children, have disproportionate exposure to air pollution66 and to the effects of climate change.67 Contributing factors include the siting of polluting sources in or near disadvantaged neighborhoods and a lack of adequate nutrition, health care, education, and social support. Risks from heat waves are greater in low-income communities of color, where discriminatory policies such as redlining have created urban heat islands (characterized by heat-trapping asphalt, few trees, dense concentration of buildings, traffic, industry, and highways) and where resources to protect children from heat are fewer.68 Similarly, disadvantaged children have been disproportionately affected by severe storms, such as Hurricanes Katrina (in 2005) in Louisiana and Harvey (in 2017) in Louisiana and Texas.69
Climate change and air pollution are exacerbating existing socioeconomic and racial and ethnic inequities in children’s health that are associated with structural racism. For example, in the United States, the preterm birth rate is more than 50% higher among Black women than among White women; for childhood asthma, the rate among Black children is more than double that among White children.70,71 Black children have had a higher rate of pediatric emergency department visits for mental health than White children.72 In a situation with global warming of 2.0°C, Black persons are approximately one third more likely than White persons to live in areas with the highest projected increases in childhood asthma diagnoses, a factor that is attributable to higher concentrations of particulate air pollution that has been linked to climate change.67 In addition, low-income children have a 15% higher projected increase in the incidence of asthma diagnoses than non–low-income children.73
Population-Level Strategies for Mitigation and Adaptation
The solutions that are briefly described in this section are largely framed as climate and environmental strategies; however, they should also be seen as essential public health policy. There is a need for simultaneous action on two fronts: to protect children today from climate hazards (adaptation) and to attack the root problem by reducing emissions of greenhouse gases and strengthening natural carbon sinks (mitigation). Adaptation measures include the provision of clean water to children and families facing drought and water contamination; early-warning systems for flooding and air pollution; disaster-response training and evacuation planning for families and children; shaded areas where children play, live, and go to school; and mosquito nets to protect children from malaria and dengue. To address inequality, these climate-specific measures must be paired with broad social programs to reduce poverty and to provide water, sanitation, hygiene services, high-quality health care, and education.
Table 2.
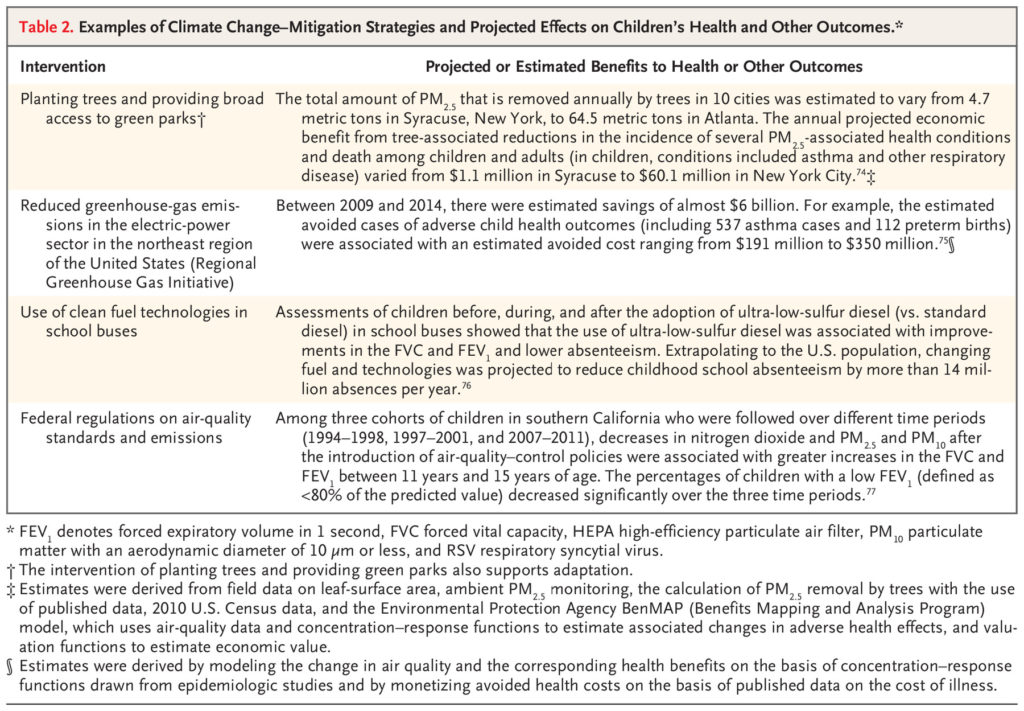
Examples of Climate Change–Mitigation Strategies and Projected Effects on Children’s Health and Other Outcomes.
Effective strategies are available and are being implemented in various parts of the world to mitigate climate change and reduce air pollution. Such strategies include federal, state, or local policies that facilitate a shift from fossil fuels to renewable energy sources, increasing energy efficiency, boosting natural carbon sequestration, and strengthening the social safety net.8 Although data from randomized clinical trials to assess the effect of such strategies on children’s health are largely lacking, data from observational and modeling studies indicate substantial projected health benefits to children and associated economic savings of some mitigation and adaptation strategies for climate change and air pollution (e.g., reducing emissions, changing to ultra-low-diesel school buses, and tree planting) (Table 2). Governmental policies that have directly targeted emissions from fossil-fuel burning can both benefit children’s health and be cost-saving. For example, between 2009 and 2014, the reduction in ambient PM2.5 as a result of the Regional Greenhouse Gas Initiative in the northeastern United States was estimated to have prevented more than 16,000 cases of respiratory illness, 537 new cases of asthma, and other illness in children, with substantial cost savings.75
Implications for Clinical Practice and Public Health
Health professionals caring for children need to understand the health harms of climate change and air pollution in order to effectively counsel children and their families on risk-reduction strategies. The American Board of Pediatrics has a Maintenance of Certification module on climate, health, and equity and is the first board to offer such content. Some medical schools and residency training programs have added curricula that address climate change–related risks among children and pregnant women; in some cases, they include opportunities to teach mitigation and adaptation techniques to the local pediatric population (see the Supplementary Appendix, available with the full text of this article at NEJM.org).
Table 3.
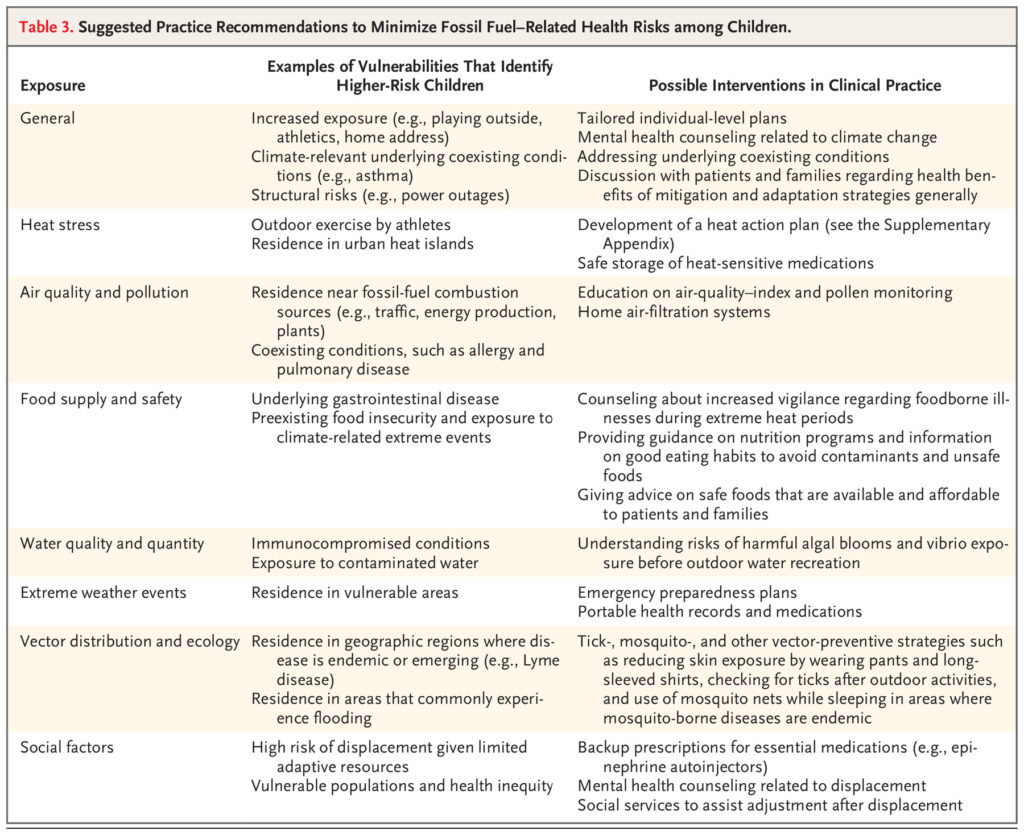
Suggested Practice Recommendations to Minimize Fossil Fuel–Related Health Risks among Children.
Guidance is available to help in identifying persons at particular risk from climate change or air pollution on the basis of assessments of underlying illness (e.g., asthma), geographic location (e.g., proximity to air pollution sources, urban heat islands, or flooding), and mental health burdens (e.g., anxiety after being forced to relocate after a wildfire) (Table 3 and S1 in the Supplementary Appendix). Given the recognition that long-term exposure to air pollution causes childhood diseases such as asthma,54 there is now a clinical code for air-pollution exposure (Z77.110) in the International Classification of Diseases, 10th Revision.
Patient-Level Interventions
Table 3 provides practical guidance for pediatricians and other health professionals caring for children with respect to screening, treatment, and counseling regarding adaptation strategies. Suggested behavioral changes need to take into account the socioeconomic status of children so that the changes are actionable and durable and empower the child and family rather than making them feel powerless, afraid, or guilty. We recommend that, in parallel with these screening assessments, health care professionals work with pediatric patients and families to implement interventions, to build their awareness of the harmful effects of climate change and pollutants, to actively motivate them to change their behaviors to protect their own health while lowering their carbon emissions, and to provide guidance on avoiding and managing various harms (e.g., heat).78
Future Needs and Directions
Climate change continues to demand better health care systems and improved access to mitigation and adaptation plans for hundreds of millions of children and pregnant women around the world. Rigorous physiological and epidemiologic data exist that link climate change with multiple effects on health. However, further research is needed in order to better understand the range of short- and long-term effects on children’s physical and mental health of climate-change pathways and air-pollution exposure (e.g., longitudinal studies to evaluate longer term effects of displacement and stress that are due to extreme climate–related events in childhood), to monitor and measure sustained health effects in children and pregnant women that have been associated with various mitigation and adaptation strategies (e.g., research into health outcomes in children in households that use only electricity, as compared with gas, for energy), and to study economic and quality-of-life outcomes (e.g., cost-effectiveness analyses that take into account reductions in hospitalizations and other medical expenses for children or pregnant women and are associated with strategies to reduce PM2.5 exposure). It is of paramount importance that research findings be rapidly translated into policies to protect and improve children’s and maternal health, with special focus on vulnerable populations.
Conclusions
The data are compelling that the toll on children and pregnant women from fossil-fuel–driven climate change and air pollution is large and growing, affecting immediate and long-term health. Interventions — which are, in many cases, cost-saving — exist to address the causes of climate change and air pollution and the disparities that they have created. Health professionals have the power to protect the children they care for by screening to identify those at high risk for associated health consequences; by educating them, their families, and others more broadly about these risks and effective interventions; and by advocating for strong mitigation and adaptation strategies.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank Dr. Vanitha Sampath and Ms. Kaitlyn Coomes for editorial assistance and reference preparation with an earlier version of the manuscript.
Author Affiliations
From the Department of Environmental Health Sciences and Columbia Center for Children’s Environmental Health, Columbia University, New York (F.P.); and the Departments of Medicine, Pediatrics, Otolaryngology, and Epidemiology and Population Health, Stanford University, Stanford, CA (K.N.).
Dr. Perera can be contacted at fpp1@columbia.edu or at the Columbia Center for Children’s Environmental Health, Columbia University, 722 W. 168th St., 12th Fl., New York, NY 10032.
Supplementary Material
| Supplementary Appendix | 157KB | |
| Disclosure Forms | 162KB |
